My 7-year-old intently looked into my eyes and asked “mama, why are there so many corona cases in our country? Isn’t our healthcare system one of the best?”
Now, what should I reply? Here he is, a 7-year-old yet well informed little person (moms of little children would understand). Nowadays, children are well-read for their age and thanks to online education and easy access to a device, they are well informed with the recent statistics. So, I cannot evade his question nor rubbish it away. Obliged to answer, I am. A reply that my generation owes the next. I have to balance carefully: not give too much information and at the same time not hide the facts.
Here is what I told him:
“Honey, no doubt our healthcare system is one among the best in the world yet we are faced with a huge wave of patients. For example, your school might be one of the best in the country but what if there were 5 times more students who joined your school. You would suddenly have 100 students in your class rather than 20. How chaotic would that be? Can your teachers handle that? Would you have enough place in your classroom? Yet you still have the best of teachers, gym, library and other buildings. So now what do you think? He started to give me possible solutions to each issue (he is a male from “MARS”, pun unintended). I simply said, “yes, darling many changes are possible but it takes time, so there will be a struggle before we can handle things”.
Here is what I didn’t tell him:
Lessons from Italy
Filippo Taddei, a Johns Hopkins associate professor of international economics and a faculty member at SAIS Europe points out that we (Europe) were a bit complacent and were not as agile as we should have been. According to Taddei, “from an economic and policy point of view, we in Italy, and in Europe more broadly, were convinced that we stood on higher ground in terms of the standards of our health system. There was a general sense that our health system, throughout Europe, was superior and more robust, which would make the virus easier to contain here in comparison with Asia. The problem is we completely underestimated how contagious and severe COVID-19 is, and the implications for our demographic structure. Moreover, we underestimated how a health system geared to address conventional health needs might be very poorly placed to deal with an epidemic”.
Earnest east
In hindsight, the key to contain COVID-19 is adequate testing to my opinion. Taiwan proactively launched a toll-free number for citizens to arrange testing, isolation and quarantine if needed, health checks, the delivery of food and the setting up of other resources. South Korea flattened the curve by extensively tracking down the contacts of the confirmed cases, which is not a straightforward measure in Europe because of the EU privacy laws.
America’s misplaced priorities
President Obama set up a pandemic preparedness office in 2016 in the aftermath of the Ebola breakout. He created the unit to prepare for future disease outbreaks and prevent them from mushrooming into pandemics. Sadly, Trump refused to learn from the experience of his predecessor and disbanded the pandemic preparedness office. Thereby compromising America’s biodefence and clearly misplacing priorities.
Practical problems in Europe
 The triage system for admitting patients into hospitals in Europe has become a discussion point among healthcare experts. This single window procedure is a conventional approach to an extraordinarily unconventional situation. So healthcare systems take a while to adapt to newer ways of mitigating this issue perhaps after a few exhausting waves.
The triage system for admitting patients into hospitals in Europe has become a discussion point among healthcare experts. This single window procedure is a conventional approach to an extraordinarily unconventional situation. So healthcare systems take a while to adapt to newer ways of mitigating this issue perhaps after a few exhausting waves.
In an article in Nejm Catalyst, a doctor clarifies “Western health care systems have been built around the concept of patient-centred care, but an epidemic requires a change of perspective toward a concept of community-centred care. Rather than containing the virus, we ended up spreading it. We learned this the hard way. We were the victims of our own successful health system in a way”.
Points to ponder:
- Why was a task force not set up already when extraordinary numbers were reported in Hubei and the rest of Asia? Or didn’t we know enough about the preventive measures? Was there a containment strategy available in the event of a pandemic?
- Testing is key because testing stops spreading. So, why was NL not ready with enough testing kits? People with mild symptoms are the most important source of contamination. If enough number of kits were available then it is possible to quarantine positive cases.
- Training programs for healthcare workers to deal with the COVID-19 pandemic could have been adroit. Did NL healthcare workers have access to such training programs?
- Why did it take so long for our Government to come up with applications to assist the identification of contacts of infected patients?
Where does the Netherlands stand at present?
Testing and apps to the rescue

Prime minister Rutte announced that testing would increase four-fold. Currently, daily testing is about 3000 to 5000. An increase to about 29,000 tests a day is expected in a few weeks. While Minister De Jong has just announced on Tuesday that they are looking into 2 apps to aid mitigation. One app helps keep track of contacts of infected cases while the other helps keep in touch with a doctor.
Stringent enforcement of the physical isolation measures is helping to ensure that citizens follow the rules. Recently, all passengers of a bus were fined €399 for violating corona measures.
Intensive care beds and expected peak
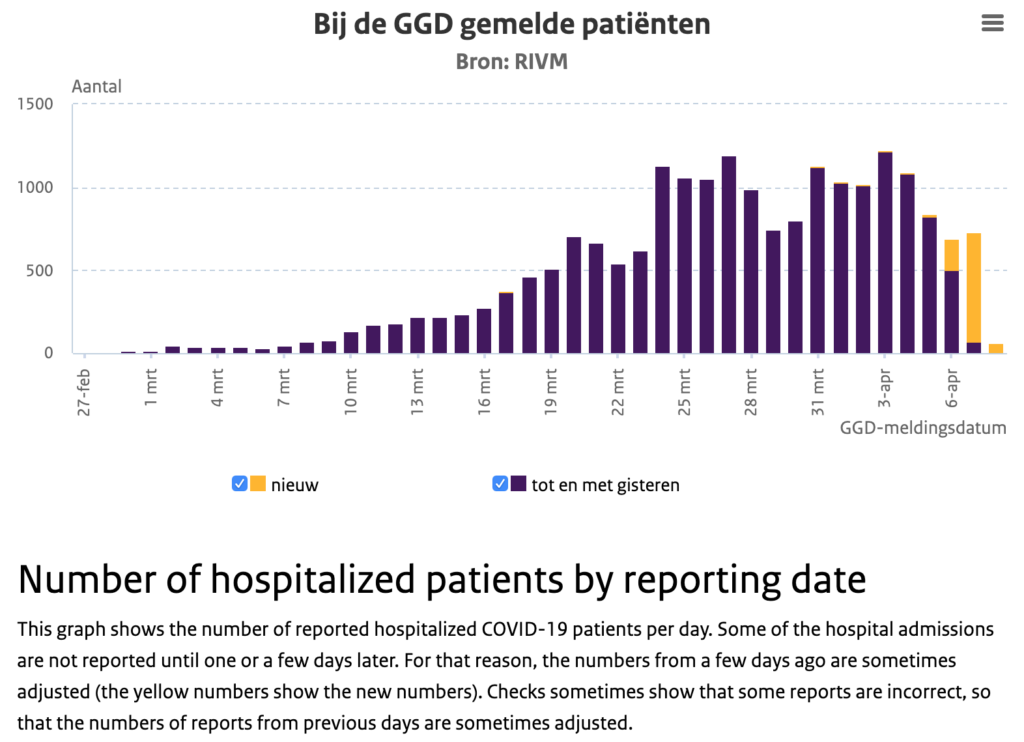
Tuesday evening, Ernst Kuipers of the Landelijk Netwerk Acute Zorg and Diederik Gommers, Chairman of the Dutch Association for Intensive Care jointly addressed the press. “We now have those 2400 IC beds available [for corona patients] and the forecast is that we will have enough in the coming weeks“, said Kuipers. He also revealed that the number of hospital admissions has been declining for the past few days. Meanwhile, Gommers cautioned “do not forget that the peak in the number of IC admissions for corona patients might be here in a fortnight“.
Who gets preference to an ICU bed?
It is quite relieving to know that we don’t have a shortage of ICU beds in the Netherlands. However, we could soon experience such a crisis. In that case, then we might face a difficult scenario of preference/priority. Would preference come based on age or a first-come, first-served basis or a draw system etc? That is not clear nor conclusive at the moment. The government-funded Center for Ethics and Health advised in 2012 to conclude who gets priority in times of scarcity (of ICU beds) during a crisis. Unfortunately, the advice did not result in action. So an ethics guideline document specifically about preference is in the making. Nevertheless, the existing guidelines for fair selection in the event of a pandemic can be found here.
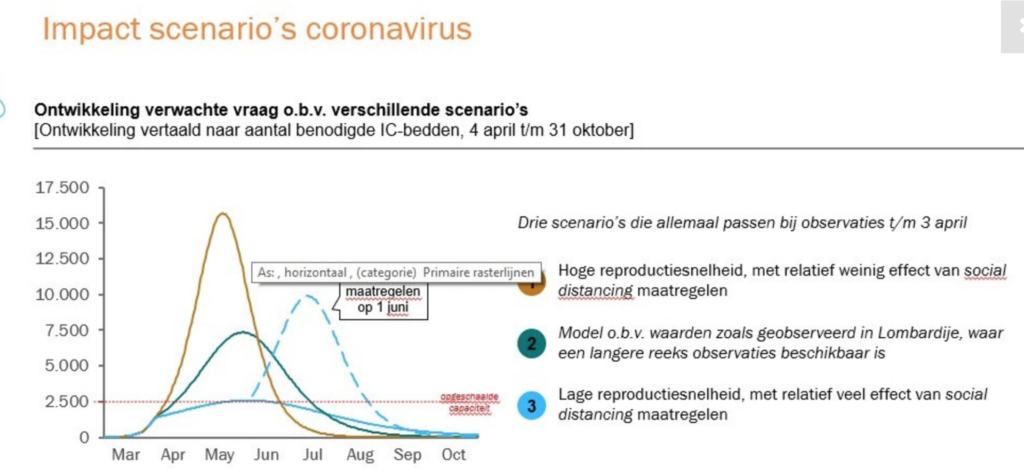
If we adhere to the social distancing measures strictly we can avert a multifold increase in demand for ICU beds. In effect, we can flatten the peak and avoid the use of “preference during scarcity guidelines”. So much to gain for staying home!
What can we do?
While the healthcare system and its overworked patrons are trying to adapt to the present crisis, we, as a society have to put forth our best efforts. In my opinion, the main responsibility would be to negate fear-mongering and shoot down misinformation. Indeed, support our Healthcare heroes and show solidarity to people running the essential services. Not to mention, we have to follow physical distancing rules and stay home. No matter how much ever the good weather beckons, we must resist the temptation.
So, how has the Netherlands managed the crisis so far?
I wouldn’t deduce the corona measures as inefficient. On the other hand, it is not only a case of grossly underestimating the pandemic but also failing to quickly adapt both as a government and as a society. Despite the staggered start: the government, public and other public bodies have upped the ante.
Children (including the little ones) need to learn from such life experiences. They understand that grown-ups can make some mistakes too. But what matters is that children realise how hard everyone tries to make life wonderful again. This is, indeed a life lesson for future generations.
For Eindhoven News: Beena Arunraj
Sources: John Hopkins University, Nejm Catalyst, USA today.
- Mirco Nacoti, MD,
- Andrea Ciocca, MEng,
- Angelo Giupponi, MD,
- Pietro Brambillasca, MD,
- Federico Lussana, MD,
- Michele Pisano, MD,
- Giuseppe Goisis, PhD,
- Daniele Bonacina, MD,
- Francesco Fazzi, MD,
- Richard Naspro, MD,
- et al











